The Differences Between Remote Patient Care Programs
How often have you, as a medical professional, wished for a more streamlined way to monitor and care for your patients outside the traditional healthcare setting?
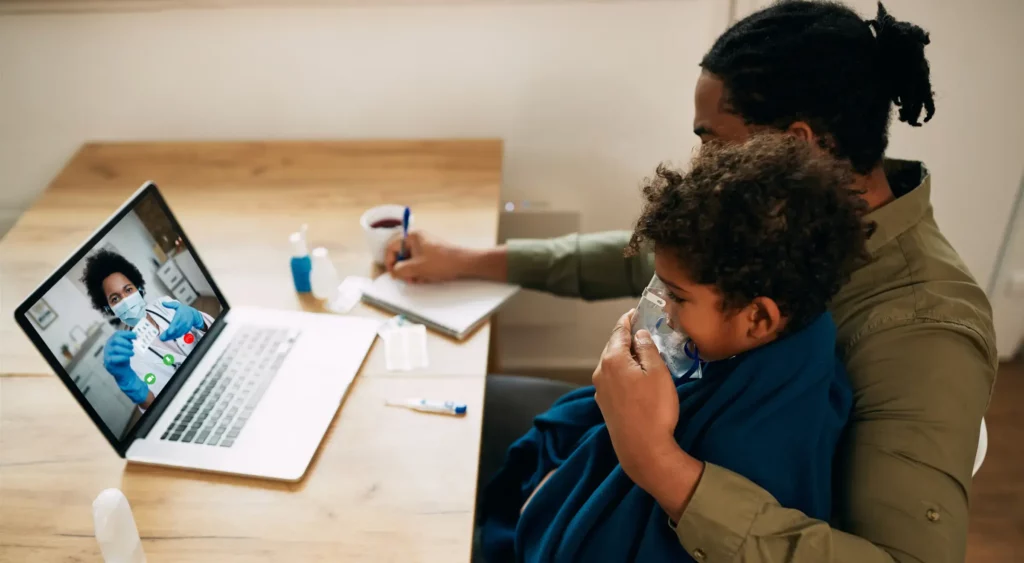
In today’s fast-paced world, where patients demand convenience without compromising quality, remote healthcare programs offer a solution. These innovative tools bridge the gap between in-person visits and enhance patient outcomes.
But with various options available, how do you discern which program aligns best with your patient’s needs? Let’s delve into the world of remote care to help you make an informed decision.
Table of Contents
ToggleUnderstanding Remote Care Programs: A Medical Perspective
Remote care programs represent the convergence of clinical protocols with advanced digital health platforms, enabling real-time biometric data collection, analysis, and intervention.
These systems leverage FDA-approved monitoring devices, secure data transmission protocols, and cloud-based analytics to view a patient’s health metrics comprehensively.
By integrating with Electronic Health Records (EHR) and utilizing predictive algorithms, remote care programs facilitate early detection of anomalies, allowing timely interventions based on evidence-based guidelines.
For care providers, this means enhanced patient monitoring capabilities, care coordination, streamlined workflows, and the ability to make data-driven decisions in a dynamic healthcare environment.
A Concise Breakdown of Remote Healthcare Programs
Drawing from extensive clinical studies and guidelines set by health authorities, here’s the overview of the primary remote care programs:
What It Is: Remote Patient Monitoring (RPM) in healthcare is a system that uses digital devices to collect health data from patients in one location and electronically transfer it to healthcare providers in a different location.
Best For: Continuous monitoring of vital signs or specific health parameters.
Example: A patient with congestive heart failure might require daily weight and blood pressure monitoring using RPM. Significant changes can trigger alerts, allowing for timely interventions and medication adjustments.
What It Is: Focuses on monitoring non-physiological data, such as a patient’s adherence to medication or therapy.
Best For Services emphasizing therapeutic adherence.
Example: A patient undergoing physiotherapy post-knee surgery might use the RTM service to report pain levels and range of motion, ensuring they progress and adhere to their therapeutic exercises.
What It Is: A service designed for patients, especially Medicare beneficiaries, with multiple chronic conditions. It aims to provide continuous care and coordination.
Best For Managing multiple chronic conditions.
Example: A patient diagnosed with diabetes and hypertension might benefit from CCM. Regular check-ins, medication reviews, and lifestyle counseling can be coordinated, ensuring both conditions are optimally managed.
What It Is: Tailored for patients with a single high-risk chronic condition, PCM integrates best practices to ensure comprehensive care.
Best For Managing a single high-risk chronic condition.
Example: A patient with a rare autoimmune disorder might require specialized care through PCM. This ensures they receive regular monitoring, medication adjustments, and access to specialists as needed.
What It Is: Focuses on the transition of patients from a hospital setting to their home or another community setting.
Best For: Post-hospitalization care.
Example: A patient discharged after a pneumonia hospitalization might benefit from TCM. This ensures they receive appropriate follow-up, medication reconciliation, and monitoring for signs of relapse or complications.
Crucial Factors Medical Professionals Should Consider for Medicare Beneficiaries
For doctors and caregivers keen on integrating remote care programs, focusing on the most impactful aspects that influence patient care and clinical operations is vital. Here are the five primary, evidence-backed considerations:
- Clinical Efficacy and Patient Outcomes: Prioritize programs with a proven track record, validated by clinical studies that enhance patient outcomes. Assure that the chosen solution aligns with the best practices of evidence-based medicine.
- Technological Reliability: Opt for programs that utilize FDA-approved or clinically validated devices. The precision of data is paramount, and trusted devices ensure that clinical decisions are based on accurate information.
- Reimbursement and Financial Implications: Stay updated on the evolving healthcare reimbursement landscape, especially for Medicare beneficiaries. Choose programs that align with current reimbursement models to ensure financial sustainability.
- Data Security and Compliance: In today’s digital health era, safeguarding patient data is crucial. Ensure the chosen program adheres to HIPAA guidelines and employs stringent encryption methods.
- Interoperability with Existing Systems: The remote care program should seamlessly integrate with existing Electronic Health Record (EHR) systems, centralizing patient data and streamlining clinical workflows.
The Ascending Role of Remote Patient Care in Modern Healthcare
Remote care programs empower caregivers with advanced tools for patient care. They enable remote monitoring, early intervention in critical health parameters, cost-effective healthcare, effective management of complex conditions, streamlined post-hospitalization care, active patient involvement, and data-driven insights for precise decision-making.
These roles equip caregivers with essential resources and cellular medical devices to provide high-quality care and improve patient outcomes.
In Summary!
For doctors and caregivers, remote care programs represent the convergence of technology and clinical care. As the medical field continues to evolve, staying abreast of these programs is not just beneficial—it’s imperative.
By integrating these programs, medical professionals can ensure they are at the forefront of healthcare innovation, offering their patients the best care possible.
Please request a free demo to learn about HealthArc’s digital health platforms can help your organization achieve its remote patient monitoring, management, and billing goals.
Most recent blogs
Categories
- Advanced Primary Care Management
- Behavioral Health Integration
- Cellular Remote Patient Monitoring
- Chronic Care Management
- Chronic Care Management Billing
- Chronic Care Management CPT Codes
- Chronic Care Management Program
- Chronic Care Management Software
- Digital Health Platform
- Principal Care Management
- Principal Care Management CPT Codes
- Remote Care Programs
- Remote Monitoring Devices
- Remote Patient Care
- Remote Patient Monitoring
- Remote Patient Monitoring Billing
- Remote Patient Monitoring CPT Codes
- Remote Patient Monitoring Devices
- Remote Patient Software
- Remote Therapeutic Monitoring
- Remote Therapeutic Monitoring Billing
- Remote Therapeutic Monitoring CPT Codes
- Telemedicine & RPM
- Transitional Care Management
- Transitional Care Management Billing
- Transitional Care Management CPT Codes
Related Posts
- May 22, 2024 | Read Time: 5 mins
Remote Patient Monitoring (RPM) For Blood Pressure Management: How It Works?
- March 23, 2021 | Read Time: 6 mins





